URINARY INFECTION IN PEDIATRICS


Glossary of Terms:
- Dysuria: Difficulty or pain in the evacuation of urine
- Enuresis: involuntary urination.
- Hematuria: Presence of blood in the urine.
- Piuria: Presence of pus in the urine.
- Polaquiuria: It is a urinary sign, a component of the micturition syndrome, characterized by an increase in the number of urinations.
- Urinary Urgency: It is the sensation of not being able to contain the urine and have the need to urinate as quickly as possible because of the risk of urinary incontinence.
Why talk about Urinary Infection in Pediatrics?
Basic Definitions:
- Urinary infection: It is the invasion, multiplication and inflammation by an uropathogen located anywhere in the urinary tract.
Bacteriuria: Presence of bacterias in the urine with or without infection of the urinary tract
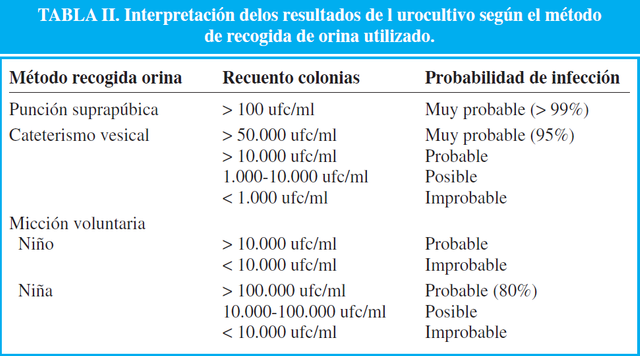
Significant Bacteriuria: Isolation of a microorganism in urine culture, more than 100,000 colony forming units (CFU / ml) by spontaneous urination, of any bacterial growth by suprapubic puncture, from 10,000 to 50,000 CFU per bladder catheter. Bacteriuria can be classified below in the history that corresponds to true infection of the urinary tract, asymptomatic and complicated.
Asymptomatic Bacteriuria: Presence of a significant count of bacteria in the urine in the absence of clinical signs or symptoms
Complicated Bacteriuria: Curses with a significant count of bacterial colonies in the urine culture in a patient with anatomical or functional alteration of base.
Now, we see that the term Urinary Infection encompasses a heterogeneous group of conditions, which what they have in common is the presence of bacteria in the urine. It can affect the urethra or bladder (low urinary tract) and the ureters, renal pelvis, calyces and renal parenchyma (high urinary tract). In this way we see that from the topographic point of view can be classified into:
- Pyelonephritis: Also known as high Urinary Infection. It is located at the level of the pyelocalic system and renal parenchyma. It is the UTI that presents fever> 38.5 ° C associated with signs of inflammation and also with systemic symptoms, such as abdominal pain, nausea, and in some cases diarrhea. It is more frequent in <2 years. Another important characteristic is that because of its location, this UTI can be complicated, since there is a risk of kidney injury with the appearance of cortical scars.
- Cystitis: Also called a low urinary infection. It is due to inflammation of the bladder mucosa. It manifests clinically with urgency, dysuria, frequency and hematuria. It is not associated with fever or systemic involvement. It occurs in girls> 2 years and usually there is no anatomical malformation base.
- Urethritis: Inflammation of the urethral mucosa. It is rare in pediatrics as an isolated entity, it is also manifested with voiding symptoms such as dysuria, frequency, secondary enuresis, pyuria without fever and, often, with elimination of exudate as seen in adolescents.
- Recurrent: With isolation of the germ after having had a sterile culture.
- Relapses: When there is persistence of the original strain in the same focus of infection, it occurs in the first weeks, and is mainly due to non-compliance with treatment, or to the use of inappropriate treatment.
- Reinfection: Isolation of a different germ after two weeks of initial treatment.
Escherichia coli: It is the main causative agent of UTI, both in girls and boys, the main route of infection being the ascending pathway, from microorganisms coming from the intestine that are in the perineal area and ascend through the urethra to the bladder. (This would explain the higher incidence in girls than boys: their urethra is shorter and gives an anatomical characteristic of susceptibility).
Other bacteria that are frequently related to the development of UI are: Klebsiella spp, Proteus mirabilis, others Grammnegative enteric bacilli, Enterococcus, Staphylococcus spp and Pseudomonas.
Urethra shorter in girls.
Children not circumcised.
Fecal incontinence and / or very prolonged exposure to the stool in the diaper.
Presence of anatomical or functional alterations of the urinary tract.
Previous diagnosis of acute pyelonephritis and recurrent previous urinary infections.
Children under two years.
Obstructive uropathy and neurogenic bladder.
States of immunosuppression.
Sexual activity or sexual abuse.
Presence of probes or catheters.
As already mentioned above, the symptoms vary depending on the location of the infection (High Urinary Tract Infections includes: high fever + touch of the general state vs Low Urinary Tract Infections include: Urinary Symptomatology as a fundamental data). This information would serve to classify and diagnose a UTI in adults without any problem, however in the case of pediatric patients, the symptomatology also varies according to age, where we must remember that the clinical manifestations are all the more nonspecific as the child is younger:
Neonatal period:
Highly unspecific. The symptomatology can range from a septic child with poor appearance, thermal instability, irritability, lethargy, rejection of food, abdominal distension, vomiting, jaundice, or various combinations of these manifestations, up to a simple weight loss, with or without anorexia, vomiting or occasional irritability. From the week of life it can already be presented as a clinical picture of isolated fever.Infants and children <2 years old:
Fever, vomiting, alteration of the depositional rhythm, weight stagnation, anorexia, malodorous urine, hematuria, abdominal pain, behavior change (irritability or apathy). It is not uncommon for the only manifestation to be a febrile syndrome without focus. In this age group, isolated cystitis is very rare.School-age children:
If it is a pyelonephritis: fever, chills, vomiting, abdominal pain, back pain, discomfort or painful sensitivity accentuated in the costovertebral angle.
When the infection is located in the lower urinary tract: dysuria, frequency, painful urination, urgency or retention, pain in the hypogastrium, enuresis; There may be, at most, a low-grade fever, and sometimes there is frank hematuria.
The clinic may suggest that a patient has a UTI, but the diagnostic confirmation is based on the laboratory study: The presumptive diagnosis is the uroanalysis, but the diagnostic confirmation requires the isolation of an uropathogen in the culture.
The American Academy of Pediatrics (AAP) recommends in infants <2 years of age who do not control sphincters, collecting urine samples for urinalysis and urine culture using two methods: suprapubic puncture and transurethral bladder catheterization.
In the following table, we can see what are the values determined for each of the methods of collection of urine that can be used in children:
The goal is to eradicate the infection, relieve symptoms and minimize the development of renal parenchymal defects.
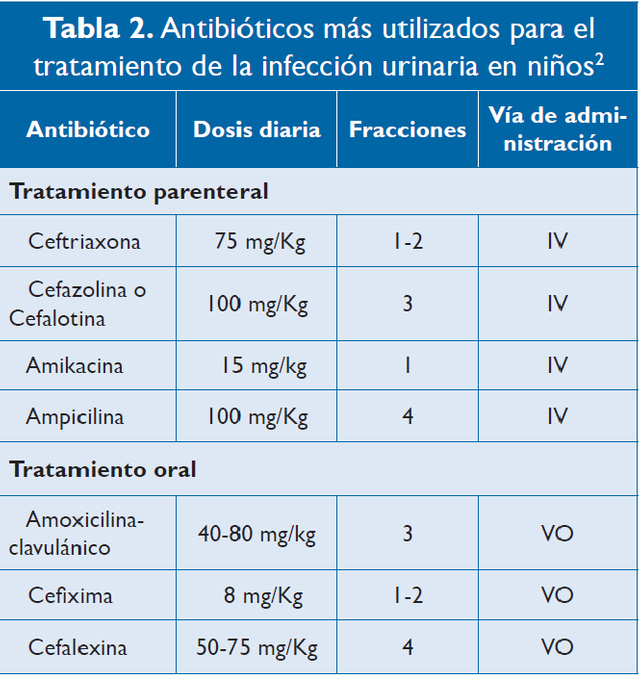
- Cystitis: Patients without systemic commitment who do not look toxic, with adequate tolerance of the oral route and reliable family and committed to care and follow-up, can be managed on an outpatient basis with oral antibiotics.
- Pyelonephritis: In infants younger than three months, feverish, toxic, with general compromise and suspicion of acute pyelonephritis, hospitalization should be made for parenteral fluid administration if required and administration of parenteral antibiotics. They should receive biotherapy with an aminoglycoside plus a penicillin; In infants older than three months, monotherapy with a first-generation cephalosporin is suggested.
The following table summarizes the antibiotics most commonly used today for the treatment of UTI in children:
It is very important to keep in mind what the Hospitalization Indications are:
- Need for parenteral antibiotic treatment, 2) Infants <3 months of age, 3) Systemic commitment, 4) Immunosuppressed patients, 5) Intolerance to the oral route, 6) Dehydration, 7) Clinical and / or analytical suspicion of Pyelonephritis at any age, and 8) In cases of non-adherence to outpatient management with difficulties in monitoring and control.*
• CONCLUSIONS:
As in any pediatric pathology, it is of vital importance to have an adequate follow-up of the patient, especially in the case of UTIs that, as already mentioned, have a high percentage of recurrences and development of complications, whether acute or prolonged over time. : Serum creatinine, urea nitrogen and the proteinuria / creatinuria ratio in a sample isolated from urine or 24 hours will be checked every six to twelve months, according to the age of the child. In ambulatory controls it is necessary to monitor blood pressure since hypertension is the most frequent complication, due to renal scars and in 10% it may present with chronic renal failure.
Hypertension, proteinuria and chronic kidney damage are consequences of late diagnosis of urinary tract infections, undiagnosed malformations and inadequate management, so it is in our hands, the health professionals, to avoid them.

I hope you liked my post, thank you so much for taking the time to read me. If you want to leave me a recommendation and / or comment, you are more than welcome! ♥ @iradyjr
https://www.fucsalud.edu.co/sites/default/files/2017-01/articulo%20revision-3.pdf
https://www.aeped.es/sites/default/files/documentos/itu.pdf
Extensive post but I think it would be better if you divide your article into a few parts; maybe for the first part discuss regarding the introduction to the disease, the next part, you can write about epidemiology, signs and symptoms etc. As most of the readers were laymen, it would be a bad idea to incorporate everything into a single article.