Hypertensive diseases in pregnancy #1
Hypertensive diseases are one of the most common medical complications during pregnancy. While I was in the clinic last week I came across a woman who was made to deliver at 25weeks because she had one of the hypertensive diseases of pregnancy. This was what prompted me to write about it.
Outline
- Definitions of terms
- Classification of hypertensive diseases in pregnancy
- Epidemiology
- Pre-ecclampsia
- Causes
- Theories
- Management
- Prevention

source
Author: Steven fruitsmask)
license>
Hypertension is defined as a systolic blood pressure (SBP) greater than or equal to140mmHg and a diastolic blood pressure (B.P) greater than or equal to 90mmHg on two occasions more than 4 hours apart
Systolic blood pressure refers to the blood pressure occurring when the heart muscles contracts
Diastolic blood pressure refers to the blood pressure during relaxation of the heart muscle.
Proteinuria
Proteinuria is defined as excretion of greater than or equal to 300mg/L in a 24hour urine sample. It could also be defined as protein measurement of 2+ or greater in at least two random urine specimen collected 6 or more hours apart. Some of the causes of proteinuria could be
- contamination by vaginal discharge,
- schistosomiasis in endemic areas,
- chronic kidney disease
- malaria.
- nephrotic syndrome
Oedema

source
Pitting oedema
James Hellman MD
Oedema in pregnancy can be said to be non-specific generalized accumulation of fluid in tissues. It can also be said to be weight gain of greater than 1 kg in any one week or 2.25 kg in any one month in a pregnant woman.
Hypertensive diseases in pregnancy can be classified as follows;
Pre-ecclampsia
Ecclampsia
Chronic hypertension
Chronic hypertension withsuperimposed pre-eclampsia
Pregnancy induced hypertension
Pre-ecclampsia It is a multisystem disorder unique to human pregnancy which is characterized by the development of hypertension accompanied by proteinuria with or without oedema, occurring in the second half of pregnancy in a previously normotensive, non-proteinuric woman.
Eclampsia This is the occurrence of fits or seizures (convulsions) in a patient with signs and symptoms of preeclampsia during pregnancy, labour or in early pueperium in the absence of an underlying neurological disease.
Chronic hypertension in pregnancy Chronic hypertension in pregnancy is hypertension occurring in pregnancy in a woman known to be hypertensive before the pregnancy, with or without proteinuria.
Chronic hypertension with superimposed pre-eclampsia This is the development of proteinuria and/or oedema during pregnancy in a patient with a history of chronic hypertension
Gestational hypertension : This is the development of hypertension in the latter (second) half of pregnancy or during labour without other evidence of pre-eclampsia or chronic hypertensive vascular disease. It is also called pregnancy induced hypertension (PIH).
Pre-eclampsia is a type that commonly occurs in the second half of pregnancy in the primigravidae. A primigravida is a woman is pregnant for the first time.It is essentially a disease of primigravidae.
This condition complicates about 2-3% of pregnancies.
It is divided into;
Mild pre-ecclampsia in which the blood pressure ranges between 140/90 – 160/110mmHg with proteinuria with or without oedema.
Severe pre-ecclampsia in which the blood pressure is greater than or equal to 160/110mmHg plus proteinuria with or without oedema.
The word eclampsia is from the Greek term for lightning.The first known description of the condition was by Hippocrates the father of medicine. It used to be call toxaemia of pregnancy.
- with Preexisting vascular disease
- with a genetic predisposition
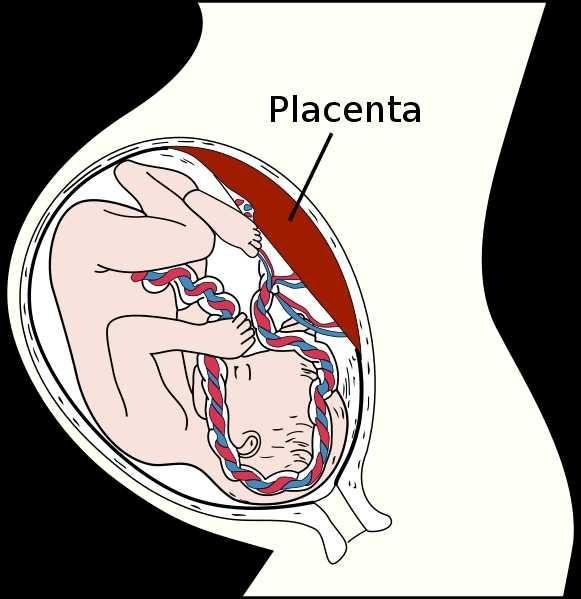
Abnormal trophoblastic invasion of uterine vessels:
Terminal uterine vessels are known as spiral arteries.
In the normal process of implantation and development of the placenta, these arteries undergo extensive remodeling as they are invaded by endovascular trophoblasts. The spiral arteries dilates so that enough blood can get to the foetus. At the end of this remodeling, the spiral artery is made of thin adventitial layer lined by trophoblasts. It is considerably dilated in diameter and is known as the uteroplacental vessel. This invasion occurs in two phases involving two thirds of the decidua. The vessels are remodeled up to the terminal resistance portion of the vessel into the myometrial layer leading to marked decrease in the resistance to blood flow into the uteroplacental vessels and into the intervillous space.As placentation progresses, trophoblastic invasion incorporates more vessels and more decidual arteries are tapped for intervillous circulation.
The invasion depth in the second-phase trophoblastic invasion might however be deficient in patients who eventually develop pre-eclampsia.The insufficient depth allows more decidual spiral arteries to retain the resistance portion of the vessel, which prevents adequate dilation of these vessels.The contractile portion of these vessels also remains intact, which has profound implication for the effect of vasomotor regulators of circulation.
This also leads to release of endothelium-damaging mediators from ischemic placenta
The result is hypertension, proteinuria and edema, plus intrauterine growth restriction (due to poor oxygen and nutrient transfer to foetus)
Immunologic theory:
There is inadequate maternal antibody response to the fetal allograft resulting in fetal allograft rejection resulting in vascular damage from circulating immune complexes in some pregnant women. It means that the woman's body recognizes the foetus as foreign.
Examples of support for this theory are nulliparous women or women who have changed their partners in subsequent pregnancies. These women have limited fetal and hence paternal antigen exposure resulting in PET.
Disseminated intravascular coagulation (DIC) theory:
There is damage to the placenta which can cause release of thromboplastin. Thromboplastin then cause disseminated intra vascular coagulopathyand fibrin deposition in the kidney and placenta resulting in development of hypertension and placental insufficiency.This is evidenced by decrease in number of circulating platelets, increase in fibrin degradation products, reduction in fibrinolytic activity observed in some cases of pre-eclampsia.
What could be a risk factor for developing Pre-ecclampsia?
Nulliparity
Multiparous with preeclampsia in previous pregnancy and/or >10 years subfertility
Multiple pregnancy
Hydatidiform mole
Diabetes mellitus
Hydropic pregnancy
Oocyte donation or donor insemination
Extremes of age (<20years and >35years)
Obesity - BMI > 35kg/m2
Family history of pre-eclampsia
New partner increases risk of re-occurence
Previously fathered a pre-eclamptic pregnancy in another woman
Prolonged exposure to paternal antigens can reoccur with the same partner at a later gestation
Pre-existing hypertension, renal disease
Pre-existing vascular disease like Collagen vascular disease
What are the signs and symptoms of pre-ecclampsia?
The manifestation of signs and symptoms would depend on the severity and progression of the disease.
There may be no symptoms especially in mild cases.
The clinical features includes;
- increased blood pressure This is a constant feature seen in this condition
- Proteinuria due to damage to the kidneys a result of deposition of fibrin and damage to the glomerulus as a result of vasoconstriction resulting in reduced blood supply to the kidneys
-Oedema (non dependent) due to reduction in oncotic pressure from loss of protein in urine.
-Brisk reflexes
-fundal height may be less than gestational age due to inadequate supply of nutrients and oxygen. This implies that the foetus has intrauterine growth restriction.
Cerebral manifestation in severe cases could manifest as headaches, dizziness, tinnitus, drowsiness,hypereflexia. This manifestation could be due to reduced oncotic pressure as a result of loss of protein in urine leading to accumulation of fluid in the brain. This fluid in the brain will then manifest with features of raised intracranial pressure.
Visual changes: blurred vision, diplopia, flashes of light, blindness. These visual changes are due to vasoconstriction in the vessels of the eye.
Gastrointestinal symptoms: epigastric pains, nausea and vomiting: due to congestion of gastric mucosa and/ or cerebral oedema
Renal symptoms: oliguria, anuria, haematuria and haemoglobinuria.
Signs of HELLP syndrome
H- haemolysis
E- Elevated
L- liver enzymes
L- Low
P- platelet count
Management
The management principles for pre-ecclampsia is aimed at:
- Control of hypertension
- Prevention of fits(convulsion)
- Safe mother followed by delivery of a live matured baby.The safety of the mother is considered first. In severe cases the fetus is sacrificed in the interest of the mother.
Since the main cause of pre-ecclampsia is in the abnormalities of the placenta, the main cure would be to remove the placenta which would imply delivery of the baby whether at term or not. The decision as when to deliver should depend on disease progression, maternal condition and gestational age. However if delivery is immediate, mode of delivery should be dependent on fetal condition and favourability of the cervix.
Most women with mild preecclamptic cases will benefit from bed rest as it is good therapy for fetal survival because it reduces blood pressure, improves utero placental flow(due to less stressful and less secretions of stress hormones) and aids fetal growth such that the fetus is matured enough to decrease prolonged neonatal intensive care admission( the closer to term delivery, the shorter the stay)
In cases of Severe preeclampsia, a wide variety of antihypertensives are used and also sedatives. Selection of the drug to use is of great importance and should be done by an expert.
The ideal antihypertensive used should be able to :-
- Lower blood pressure effectively,predictably and permanently
- Ensure fetal growth and well being by increasing utero placental blood flow
- Reverse renal vascular spasm and prevent pathological changes
- Be safe and free from side effects to mothers and babies
- Be convenient to use with reasonable margin of safety
The drugs that can be used include;
- Labetalol
- Magnesium sulfate
- Hydralazine
- Methyldopa
- Nifedipine
- Diazepam
Clinical assessment of fetal well being such as symphysiofundal height daily or twice weekly, cardotocogragh (CTG),daily fetal kick chart,serial ultra sound scan should be done and if there is fetal compromise or worsening of disease, the baby should be delivered.
What are the complications of pre-ecclampsia?
Complications of pre-ecclampsia can be divided into maternal complication and foetal complications.
Maternal complications
- Convulsions and coma (Eclampsia)
- Cerebral haemorrhage
- Stroke
- DIC
- Acute renal failure
- Hepatic Failure
- Liver rupture
- HELLP
- Encephalopathy
- Abruptio placentae
- Residual chronic hypertension in about 1/3 of cases
- Recurrent pre-eclampsia in next pregnancies
- Maternal mortality
Foetal complications
- Intra uterine growth restriction (IUGR)
- Oligohydramnios
Placenta infarcts
- Uteroplacental insufficiency
- Prematurity and its complications
- Still births
- Neonatal deaths.
What are the ways of preventing pre-ecclampsia?
The aetiology is diverse, therefore prevention is difficult. However, here are some preventive measures below
-Low dose aspirin is known to help if given to women at high risk of pre-eclampsia after 12weeks of gestation.
- Calcium supplementation
- Anti-oxidants like Vitamins C and E
What is the outcome of pre-ecclamptic women after delivery?
Studies have shown that complications tend to correlate with the age of the patient and severity of the disease. It has also been observed to recur in women with chronic hypertension.
References
- Obstetrics by ten teachers nineteenth edition
- Textbook of obstetrics and gynecology
- wikipedia
- All pictures are free source pictures from wikipedia and free to use .
Thank you for reading.
**I remain @bhoa and I intend spreading the gospel of health through the steemit blockchain... **
Steemstem is a community that supports science, technology, engineering and mathematics. Clickhere to join.
Click here to join @steemrepo.
Hi, @bhoa, There were a few typos but overall it is an average educational article. For example, putting oedema (supposed to be "pitting oedema") etc. The definition that has been given by you regarding hypertension is a theoretical definition,
In clinical settings, sometimes, people started to show symptoms related to hypertension even if their systolic blood pressure were slightly above 120 mmHg. The most important thing to consider is the mean arterial pressure (MAP). Great effort. Kudos.
Congratulations!,@bhoa Your post has been upvoted by @reachout
Our goal is to support Minnows on Steemit.
Join our discord group https://discord.gg/NWAkKfn
Major Upvote Sponsor : @bleepcoin
SP Donation by @rufans & @solomon158
Join Our Trail here: https://steemauto.com/dash.php?i=15&id=1&user=reachout
Well done @bhoa! You successfully guessed the match result.
Click on the badge to view your Board of Honor.
Do not miss the last post from @steemitboard!