This is what depression is made of! - The biological underpinnings of depression
"Hey you have fever, why don't you just lower your temperature and hang out with us!"
Now, that is not something you tell a person who has fever. But doesn't it sound familiar? Something you were told if you ever suffered clinical depression, or something you told someone who had clinical depression?

The biological underpinnings of depression
Sketched by @scienceblocks | Originally shared in my facebook
I mean the utter disregard of fact that depression is a disease that arises from body's physiology, is ridiculously huge. I mean think about it, thoughts and feelings don't arise in thin air. They have certain physiology associated with it. Everything that happens around you has an effect on your muscle tension, your heart rate, your hormones, and your neuronal firing. The sum of it makes up the feelings or emotions.
The pathology of depression
Sadness, grief and depression are inherently different in their details, nonetheless they all have underlying physiology associated with them. (Be it the physiology of your brain, body or just hormones going nuts). The physiology of depression is nonetheless pathological and it's pathogenesis is the motive of this post.
If you were to peek inside the brain of a person suffering from depression, the more you zoom in the more differences you will find in comparison to a healthy person. For instance, even if you were to take rodent model for depression used in lab, you will see that their depression like behaviour is associated with changes in dendritic spines. (For those who don't know dendritic spines are extension of membranes on neurons that receive signal from previous neuron at synapse). So depressed animals have more dendritic spines in amygdala(the fear center) and nucleus acumbens(this part of your brain is famous for anticipating the rewards). However, they have decreased density and altered morphology in hippocampus(the learning and memory center)(Qiao et al., 2016). In fact even humans suffering from depression show reduced hippocampal volume.
Pathogenesis of depression
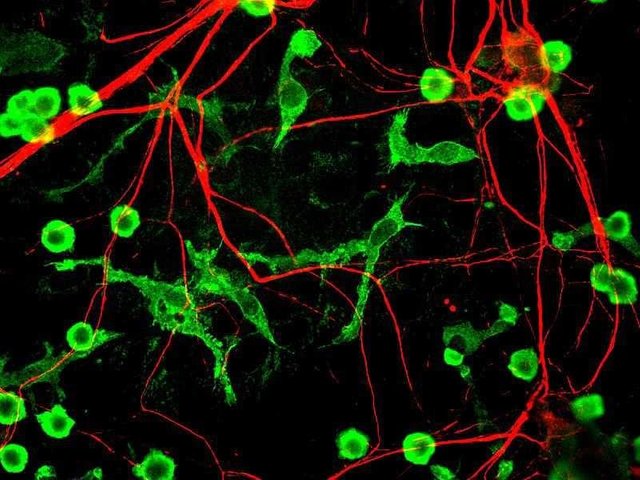
Microglia(green) cells, the immune cells in brain
Source
Author - GerryShaw
CC BY-SA 3.0
Then not only do you have altered brain physiology associated with depression, but the pathogenesis of depression itself has your immune system contributing to it. For instance the set of stress response pathways in body, that regulate the fight or flight response during those rough life situations, also seem to activate the innate immune system in body. You can find the NfKb signalling activated and these immune cells secreting inflammatory cytokines in response to stress. It is not clear why your body has to start fighting pathogens in response to psychological stress but there are a few hypothesis out there if you want to read(see Miller and Raison, 2016). I think it might just be an ancient evolutionary adaptation. Unlike most humans who get stressed just by thinking about price of Steem falling, animals get stressed when they are being chased by predators, or by social defeat from a more dominant competitor. I think it would make sense to turn on immune system after that fight for life. I mean what if you survived but that wolf left an infection in your body with that bite?
Take an example of people undergoing treatment for chronic hepatitis infection. They receive an inflammatory cytokine, interferon-alpha for treatment. Now, the interferon is generally known for killing the virus infected cells. But other than that it is also famous for clinically induced depression. Brosini et al, published this year, where they did in vitro experiments to show the mechanism behind this. They claimed that this effect is mediated by Inferferon-alpha stopping neurogenesis in hippocampus and by killing existing cells as well.
Since, this was an in-vitro study(that is it was done on cultured cells and not mice), I would have just ignored it. But then last month Nie et al., published in Neuron and made the chronic inflammation and depression link more convincing. They show that repeated social defeat stress activates Toll like receptors(TLR) in microglia of prefrontal cortex in mice. The microglia then showed increased expression of inflammatory cytokinesis such as TNF-alpha. And if you made a genetically modified mice without TLR, the mice did not develop depression like symptoms. (If you are lost then prefrontal cortex is part of brain that mostly controls social interaction. Microglia has brain's immune compartment consisting of resident macrophages. TLR are receptors on macrophages that usually bind to bacterial patterns such as lipopolysaccharide.)
Now if you know a bit of a history of depression and inflammation you may ask then what about lymphopenia(decrease in number of lymphocytes), that is associated with depression in humans. On one hand you have weak immune system with less lymphocytes and on other hand I am telling you that chronic inflammation in brain is cause of your depression. Well along with Nie et al., there was yet another interesting paper published last month by Laumet et al.,. The paper highlighted that T lymphocytes are rather important in resolution of this inflammation. They show that Rag1 null mice, which lacks adaptive immune system and hence T lymphocytes, infact has worse depression like symptoms.
The non-psychological pathologenesis of depression?
Finally, in my previous blog about Type 2 diabetes, I highlighted the role of obesity and gut microbiome in causing low grade inflammation in body. In fact I even talked about TLR signalling by bacterial LPS and free fatty acids causing inflammation in hypothalamus, that can cause compulsive eating. Now gut microbiome has been linked to causing depression and anxiety, as well(See Evrensel and Ceylan, 2015). Which makes me wonder if depression always has psychological stress at its basis or sometimes it could be triggered by other physiological conditions? What about autoimmune disorders. What about people with HLA B27 variant who suffer from ankylosing spondylitis? How much of their depression is contributed by rouge immune cells secreting TNFalpha? I think this is totally worth exploration.
So next time if you are depressed, and someone tells you why can't you just be happy, do show them the research articles mentioned here. In case they still act thick ask them that why can't they just be intelligent.
References
Signing off
@scienceblocks
Hi @scienceblocks!
Your post was upvoted by utopian.io in cooperation with steemstem - supporting knowledge, innovation and technological advancement on the Steem Blockchain.
Contribute to Open Source with utopian.io
Learn how to contribute on our website and join the new open source economy.
Want to chat? Join the Utopian Community on Discord https://discord.gg/h52nFrV
This post has been voted on by the steemstem curation team and voting trail.
There is more to SteemSTEM than just writing posts, check here for some more tips on being a community member. You can also join our discord here to get to know the rest of the community!
There are many different pathways that can lead us to depression, and I like the way you addressed how our neurobiology can be one them @sienceblocks.
The changes in dendritic spines seen in animal models you brought up here reminded me of a study I came across a while ago by Mitra and Sapolky (2008), who injected high doses of corticosterone in rats for one day to represent intense stress. After 12 days they saw that the rats had sprouted more dendrites in their amygdala neurons than the controls. This was sufficient to produce long-term anxiety and depressive behaviour. Which leads me to take into consideration the influence the social-environment might play in also giving rise to the condition discussed.
Thank you for sharing this post with us. I was looking forward to it and it has been an interesting read. Now, I am going to look into Nie et al's study. As of late, I have been going through materials that explore the association between mental-illnesses and inflammation :) as I mentioned to you before.
All the best to you :)
Take care!
Oh Spolsky's paper, I remember citing that in my Rotation project back in 2012. I was trying to understand, the effect of traumatic stress on pre existing and post trauma fear memories. For most part of my rotation I kept thinking that corticosteroids are immune suppressants. So I might have imagined that effect of corticosteroids on neurons regulate dendritic spines while it's suppression of immune system makes us more prone to diseases. But then new evidence emerged, esp in its relation to microglial cells. It appears that whether it activates the immune fiction or suppress it there depends on its dose, timing and duration. So here is an added line of inflammation, stress endocrinology and psychiatric diseases that may interest you. I think there is a lot in this field to talk about.
And once again thanks for stopping by , reading and appreciating.
Congratulations,
you just received a 19.02% upvote from @steemhq - Community Bot!
Wanna join and receive free upvotes yourself?
Vote for
steemhq.witnesson Steemit or directly on SteemConnect and join the Community Witness.This service was brought to you by SteemHQ.com