From yourself: Bone Graft
Bone Graft
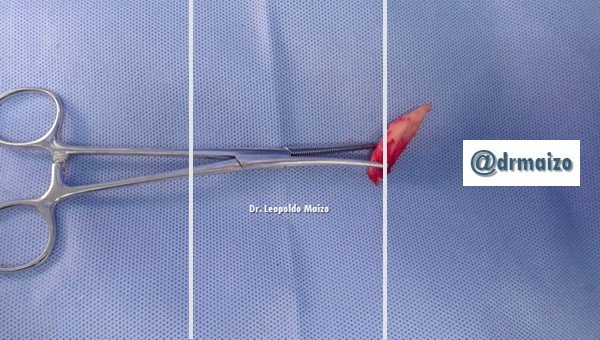
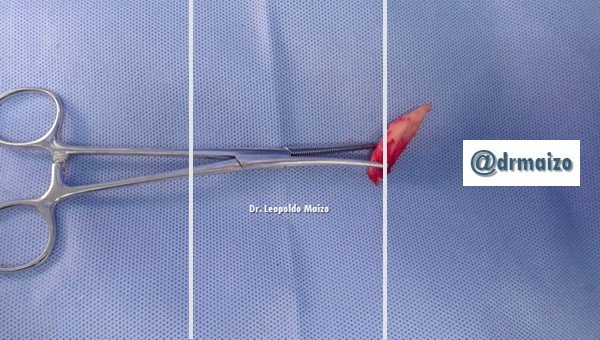
A short time ago we performed a hand surgery where we had the need to use autologous bone graft, i.e. graft from the same patient. In his case we obtained it from the iliac crest, a very common and usual area to obtain a graft. For the vast majority of patients who need it in surgeries is very beneficial because you have no additional costs for the purchase of synthetic material or cadaver, on the other hand there is no risk of adverse reaction because it comes from your own body, perhaps the only drawback is the pain that produces then and a small scar. Some cases need more graft than can be extracted so it is necessary to buy it but thanks to these cases it is possible to make comparative studies that I would like to take with me and discuss with the master surgeons who await me in Europe.

Historical data


The first indication of the use of bone grafts for the reconstruction of bone defects dates from 1668, when Van Meekren transplanted heterologous bone from a dog to man to restore a defect in the skull. In 1809 Merrem performed the first successful autologous bone graft transplant. In 1878 Macewen reportedly successfully transplanted allogeneic bone into humans. In 1891 Bardenheur was the first to perform an autologous bone graft to the mandible. In 1908, Payr described the use of free tibia and rib transplants. In 1938 Orell produced a bovine bone graft material through the use of strong alkalis, and in 1942 Wilson created a bone bank using freezing techniques.
Bone grafts are used in practically all aspects of reconstructive orthopedic surgery and range from the treatment of fractures to complex techniques of limb salvage in tumoral surgery. With respect to spine surgery, in the United States 289 thousand procedures are performed annually in which a bone graft must be placed.



Classifications
According to the results obtained from these investigations, the current classification of grafts according to their origin and structure was carried out, with the purpose of establishing some of their most important characteristics, which allow the surgeon to make the adequate choice based on the structural and functional needs required. According to these criteria, the grafts have been classified into:
- Autologues (autografts): this type of graft is composed of tissue taken from the same individual, and provides better results, since it is the only one that complies with the 3 mechanisms of bone regeneration (osteogenesis, osteoinduction and osteoconduction), it also avoids the transmission of diseases and immune rejection.
- Homologues (allografts): consist of tissue taken from an individual of the same species, not genetically related to the recipient, has osteoinductive and osteoconductive capacity, and according to Betts "behaves as a structure that will allow bone neoformation from the gradual replacement that suffers the graft by the host bone, making this process slow and with considerable loss of volume. There are 3 types of bone allografts: frozen, dried (lyophilized) and demineralized.
- Isogenic (isograft): composed of tissue taken from an individual genetically related to the recipient individual.
- Heterologists (xenografts): they are composed of tissue taken from a donor of another species, in addition clinically they are not acceptable due to their great antigenicity.

In terms of their structure, bone grafts can be: cortical and spongy; each has certain characteristics and qualities. The cortical structure produces a good mechanical filling due to its composition, since it can be easily adapted and contoured. For its optimal function it must be correctly fixed to the receptor bed, by means of plates or screws under pressure; the spongy structure fuses more quickly to the receptor bed due to the fact that the large open spaces that it presents, allow a rapid revascularization propitiating the bone neoformation; however, it has certain limitations, since it does not have sufficient mechanical resistance to tolerate tensions in defects of great size. It is for this reason that the natural union of a cortical and spongy sheet provides better results placing the trabecular portion against the host and the cortical towards the external surface. However, other varieties of bone grafts have been considered, such as: marrow, particles, and bone paste, among others.
Bone grafts are the only ones that have the particularity of naturally inducing the process of bone regeneration, which occurs from these 3 basic mechanisms:
- Osteogenesis: depends exclusively on the survival of the transplanted cells, mainly the preosteoblasts and osteoblasts. It originates mainly in spongy bone, due to its rapid revascularization, which can be complete after 2 weeks, while in the cortex it can take several months.
- Osteoinduction: it is initiated by means of the transformation of undifferentiated mesenchymal cells perivascular of the receptor zone, to osteoforming cells in the presence of regulating molecules of the bone metabolism. Within these molecules, the group of morphogenetic proteins stands out, but there are also a series of other proteins involved in bone metabolism. The source of these proteins are autologous grafts, plasma rich in growth factors and morphogenetic proteins obtained through genetic engineering techniques. The morphogenetic protein, which is derived from the mineral matrix of the graft, is reabsorbed by the osteoclasts and acts as a mediator of osteoinduction; this and other proteins must be removed before the onset of this phase, which begins 2 weeks after surgery and reaches a peak between 6 weeks and 6 months, to decrease progressively afterwards.
- Osteoconduction: it is a slow and prolonged process, where the graft has the function of skeleton. This type of healing predominates above all in cortical grafts, where the graft is progressively colonized by blood vessels and osteoprogenitor cells from the recipient area, which slowly reabsorb it and deposit new bone.

The use of bone grafts as an alternative for the reconstruction of bone defects, whether congenital or caused by trauma, oncological or infectious sequelae, are aimed at restoring the anatomical and functional integrity of an altered structure. For decades, researchers have been given the task of finding in the grafts certain characteristics that respond to each of the reconstruction needs; this fact has led to study and compare the benefits of some potentially donor bone structures, which increase the chances of successful treatment and considerably reduce the possible risks and complications during the taking of the graft. Similarly, various implant materials have been studied, however, these do not have the natural ability to induce the process of bone regeneration, making them biocompatible inert materials "filler", which do not replace the characteristics of the grafts, but used together if required, can improve the results.

If you need recommendations or help in orthopedic surgery and traumatology do not hesitate to contact me.
Dr. Leopoldo Maizo - Orthopedic Surgeon
If you want to read more I invite you to visit my page:

Firma diseñada por @themonkeyzuelans, contáctalos vía Discord "themonkeyzuelans#9087"
Great projects from the Steemit community:
- My Fundition campaign: https://fundition.io/#!/@drmaizo/6f88ggj8h


.png)
This project is being supported by @Fundition
Fundition is a next-generation, decentralized, peer-to-peer crowdfunding and collaboration platform, built on the Steem blockchain.
#upfundition and #fundition tags on Steem represent the projects that are started on https://fundition.io.
Are You Prepared to Make the World a Better Place too?
Read the full details of Fundition Fund program
Learn more about Fundition by reading our purplepaper
Join a community with heart based giving at its core
Thank you
Do you have to go back in to remove that or is it permanent?
Hi @jmehta, when you place any type of bone graft is never removed, since almost everything is reabsorbed by the body and our body begins to create new bone where this graft existed (osteoinduction). In the end you will have bone created by yourself in all cases! :D