Metastasis and cancer #2
Metastasis and cancer #2
I wanted to let you know that I’ve personally commissioned all the images you will find in this post, I released them to the public domain, thus you are free to use them. I only ask you the courtesy to copy/paste the figure legend citing the artist that drew them and the commissioner (me). If you would like to commission yourself images for science, you can find out how here
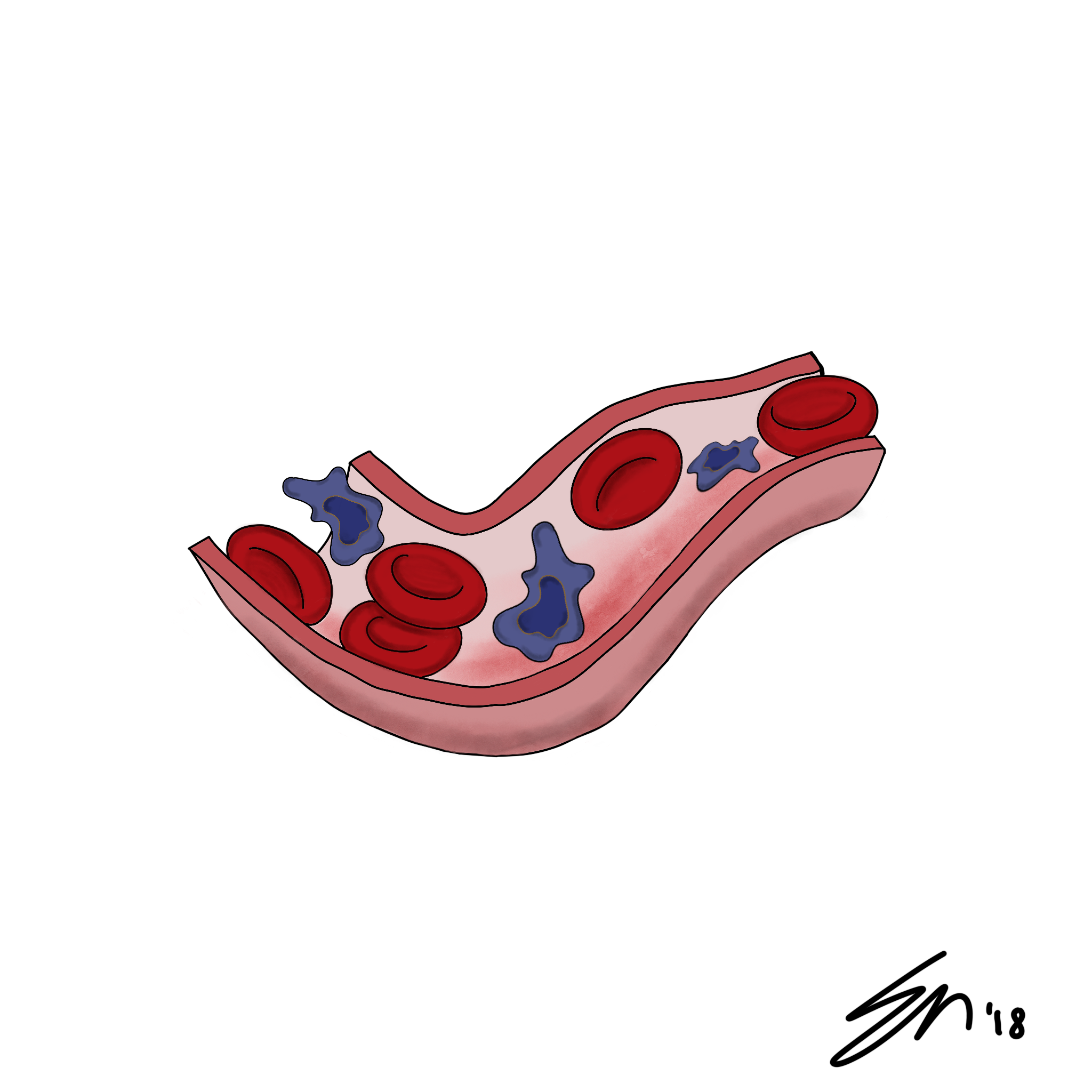 Attribution-ShareAlike CC BY-SA by @enmaart thanks to @aboutcoolscience and @davinci.art - [Source](https://steemit.com/@davinci.art)
Attribution-ShareAlike CC BY-SA by @enmaart thanks to @aboutcoolscience and @davinci.art - [Source](https://steemit.com/@davinci.art)
 Attribution-ShareAlike CC BY-SA by @enmaart thanks to @aboutcoolscience and @davinci.art - [Source](https://steemit.com/@davinci.art)
Attribution-ShareAlike CC BY-SA by @enmaart thanks to @aboutcoolscience and @davinci.art - [Source](https://steemit.com/@davinci.art)In my last post I discussed how most deaths associated to cancer are caused by metastasis. I have also provided you with an overview of the main stages of the process. Today I want to focus on a critical step: to originate a metastasis, cancer cells have to survive a brief period in circulation, we are talking of just few minutes. It may not sound much, but generally this time is sufficient for our defenses to eliminate pathogens and cancer cells unless they devised strategies to elude our defenses. Unfortunately, there are truly ingenious mechanisms that cancer cells exploit to turn our defenses against us, and not only survive in circulation, but get our immune system to help them colonize a new tissue and form a metastasis.
How cancer cells exploit interaction with platelets
I just gave you a hint earlier that cancer cells probably would not be able to survive on their own in circulation, however, they exploit circulating cells such as macrophages and granulocytes to facilitate the process of extravasation. But, there is another interaction that enable cancer cells to survive in circulation for longer, I am talking about their ability to bind to platelets gaining several advantages. First of all, it was found that metastatic cancer cells express high levels of proteins and other adhesion molecules capable of binding platelets. For example they secrete tissue factor (TF) and P-selectin ligands that also activate the platelets (Labelle, Begum, and Hynes 2014). So, what are the advantages for cancer cells?
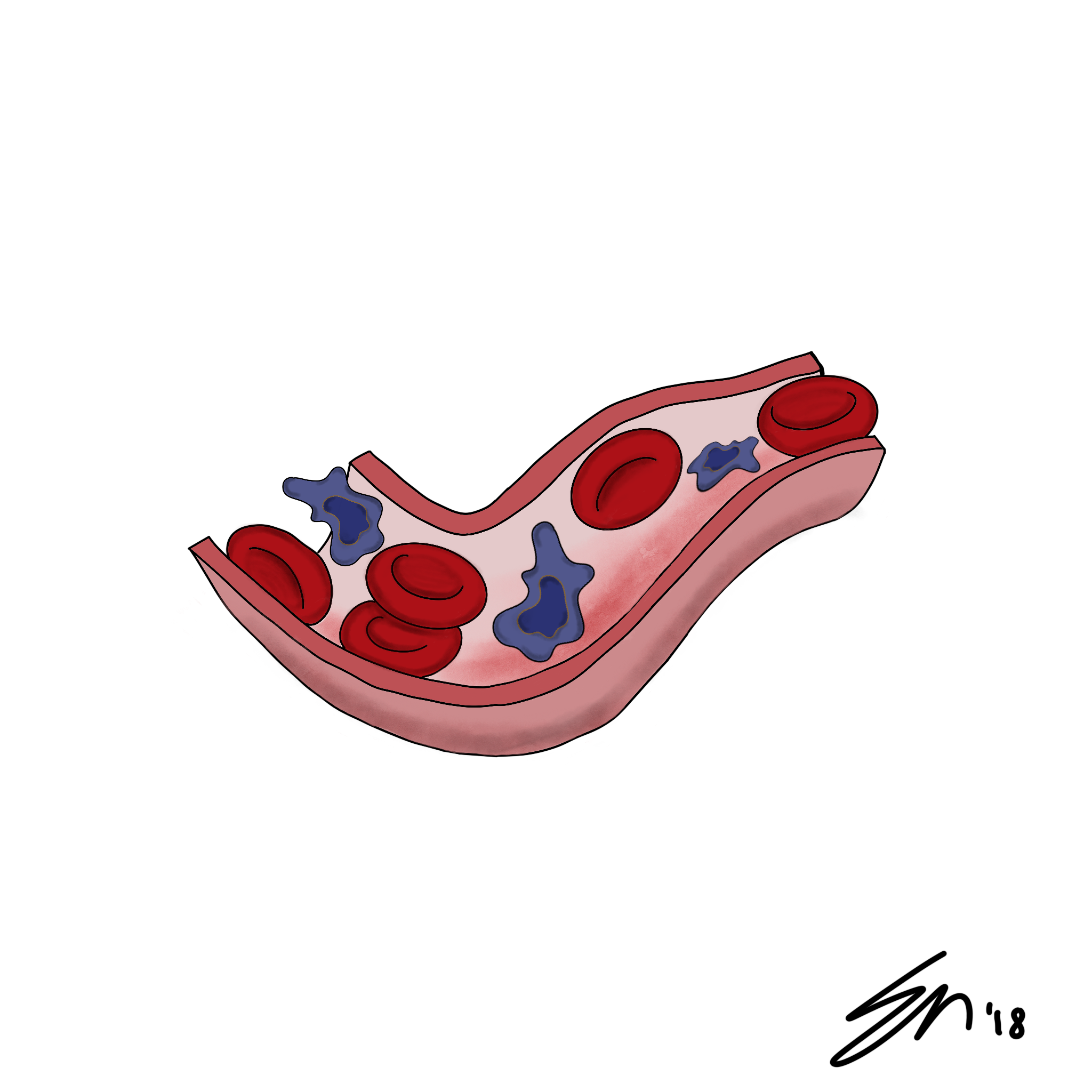
 Attribution-ShareAlike CC BY-SA by @acquarius30 thanks to @aboutcoolscience and @davinci.art - [Source](https://steemit.com/art/@davinci.art/sketches-cards-acquarius30-n-07-blood-vessel)
Attribution-ShareAlike CC BY-SA by @acquarius30 thanks to @aboutcoolscience and @davinci.art - [Source](https://steemit.com/art/@davinci.art/sketches-cards-acquarius30-n-07-blood-vessel)All the platelets that surround the cancer cells form almost a physical shield that not only hides cancer cells from the attacks of natural killer cells (NK) but also facilitates the adhesion of the tumor cells to the epithelium, thus increasing the changes of extravasation. I’ve also said that as a result of the interaction with cancer cells, the platelets can become activated thus release growth factors that could boost the metastatic potential of cancer cells. All this messing around with platelets can also alter the homeostatic controls of coagulation. This is the reason why several patients with cancer are also affected by diffused microthrombi (Gay and Felding-Habermann 2011). The interplay between cancer cells and platelets is not a novelty, already in the 1960s we realized that there was a link with thrombocytopenia (low number of platelets in circulation) and an anti-metastatic effect (Gasic, and Stewart 1968) while on the other hand, abundance of platelets was often correlated with the insurgency of metastasis (Gay and Felding-Habermann 2011). Furthermore, it was found that the tumor cells, by activating the platelets can also elicit the secretion of ATP that binds to the receptors P2Y2 expressed by the endothelial cells and causes an increase in the permeability of the vasculature, thus easier extravasation (Schumacher et al. 2013).
Inflammation and cancer
I’m oversimplifying here but studies found a correlation between postsurgical infections and the insurgency of metastasis (Cools-Lartigue et al. 2013). This is a very important finding considering that in the 2012 alone, most of the 2 million American patients diagnosed for cancer had to undergo surgery within the year (Siegel, Naishadham, and Jemal 2013) and that the incidence of postsurgical infections is around 40% (Itani et al. 2006). How?
Well, it seems that circulating tumor cells can interact with another cell type: the neutrophils, which are the first cell type to get involved in case of infections. Before delving too deeply in how cancer cells exploit neutrophils let’s first familiarize with the concept of neutrophil extracellular traps (NETs). We recently discovered that when neutrophils sense the presence of a pathogen they can extrude structures of DNA that resemble nets which are decorated with proteins having antimicrobial activity (Cools-Lartigue et al. 2013).
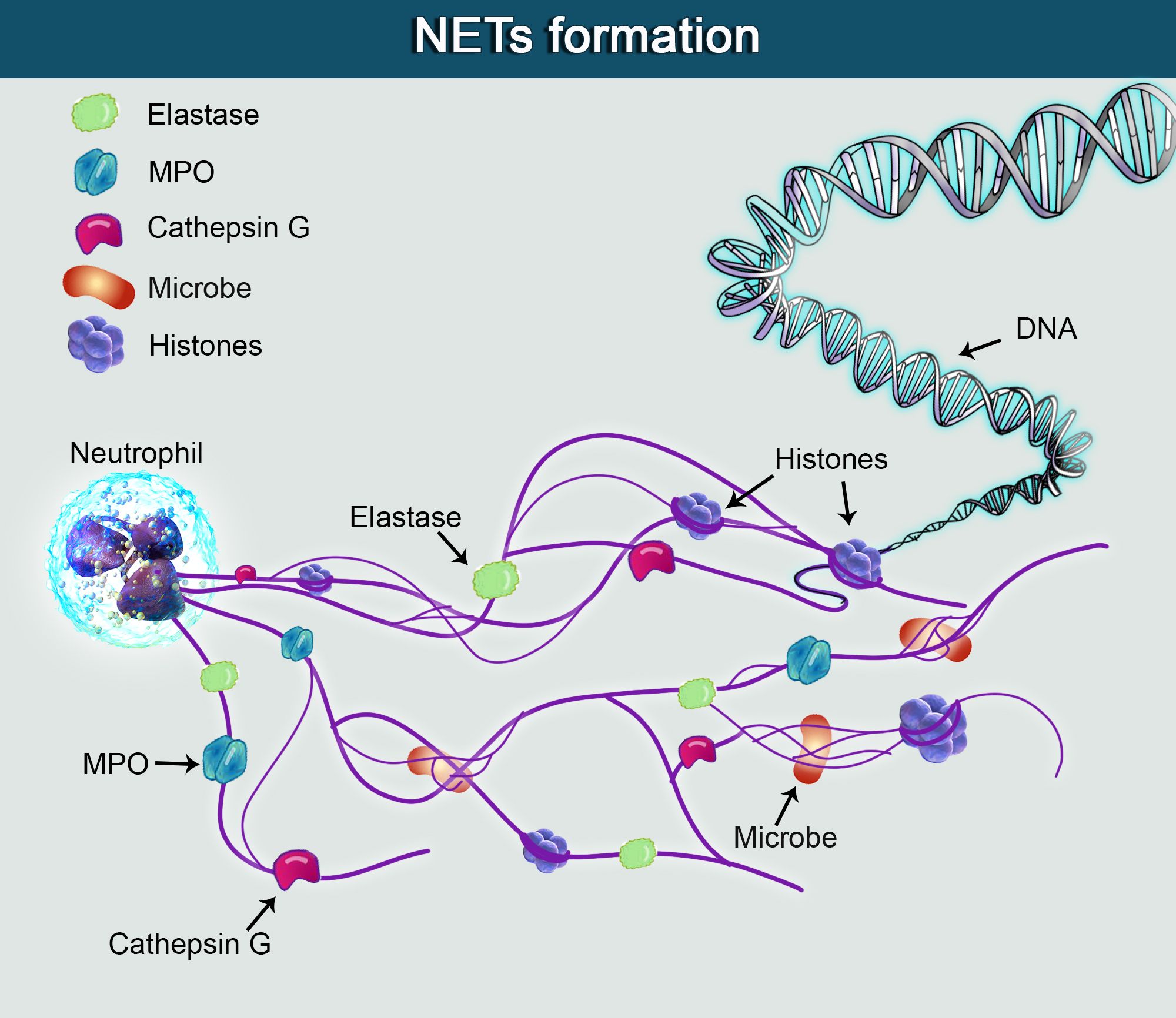 Attribution-ShareAlike CC BY-SA by @elvisxx71 thanks to @aboutcoolscience and @davinci.art - [Source](https://steemit.com/@davinci.art)
Attribution-ShareAlike CC BY-SA by @elvisxx71 thanks to @aboutcoolscience and @davinci.art - [Source](https://steemit.com/@davinci.art)As you can imagine these NETs trap and kill the pathogens. Cancer cells are very resourceful, not only they can survive to the entanglement in these NETs, but they can also use them to adhere to the endothelial cells and extravasate. Thus neutrophils seems to facilitate the adhesion of cancer cells which can dock in close proximity to endothelial cells (Spicer et al. 2012). Furthermore, neutrophils secrete also metalloproteinases that can break-down some of the extracellular matrix proteins and thus promote the extravasation of cancer cells (Spiegel et al. 2016). Also, do you remember the platelets bound to the surface of cancer cells? Well, after their activation they can also release chemokines that attract more neutrophils, increasing the chances for metastasis (Labelle, Begum, and Hynes 2014). In the next post we can discuss more details about the extravasation process.
References
Cools-Lartigue, Jonathan et al. 2013. “Neutrophil Extracellular Traps Sequester Circulating Tumor Cells and Promote Metastasis.” The Journal of clinical investigation. http://www.ncbi.nlm.nih.gov/pubmed/23863628.
Gasic, G J, T B Gasic, and C C Stewart. 1968. “Antimetastatic Effects Associated with Platelet Reduction.” Proceedings of the National Academy of Sciences of the United States of America 61(1): 46–52. http://www.ncbi.nlm.nih.gov/pubmed/5246932.
Gay, Laurie J, and Brunhilde Felding-Habermann. 2011. “Contribution of Platelets to Tumour Metastasis.” Nature reviews. Cancer 11(2): 123–34. http://www.ncbi.nlm.nih.gov/pubmed/21258396.
Itani, Kamal M.F. et al. 2006. “Ertapenem versus Cefotetan Prophylaxis in Elective Colorectal Surgery.” New England Journal of Medicine 355(25): 2640–51. http://www.nejm.org/doi/abs/10.1056/NEJMoa054408.
Labelle, Myriam, Shahinoor Begum, and Richard O Hynes. 2014. “Platelets Guide the Formation of Early Metastatic Niches.” Proceedings of the National Academy of Sciences of the United States of America 111(30): E3053-61. http://www.ncbi.nlm.nih.gov/pubmed/25024172.
Schumacher, Dagmar et al. 2013. “Platelet-Derived Nucleotides Promote Tumor-Cell Transendothelial Migration and Metastasis via P2Y2 Receptor.” Cancer cell 24(1): 130–37. http://www.ncbi.nlm.nih.gov/pubmed/23810565.
Siegel, Rebecca, Deepa Naishadham, and Ahmedin Jemal. 2013. “Cancer Statistics, 2013.” CA: a cancer journal for clinicians 63(1): 11–30. http://www.ncbi.nlm.nih.gov/pubmed/23335087.
Spicer, Jonathan D et al. 2012. “Neutrophils Promote Liver Metastasis via Mac-1-Mediated Interactions with Circulating Tumor Cells.” Cancer research 72(16): 3919–27. http://www.ncbi.nlm.nih.gov/pubmed/22751466.
Spiegel, Asaf et al. 2016. “Neutrophils Suppress Intraluminal NK Cell-Mediated Tumor Cell Clearance and Enhance Extravasation of Disseminated Carcinoma Cells.” Cancer discovery 6(6): 630–49. http://www.ncbi.nlm.nih.gov/pubmed/27072748.
Communities that support me are:
enlarge
Attribution-ShareAlike CC BY-SA
Reuse this image by copying and pasting this text with it:
Attribution-ShareAlike CC BY-SA by @elvisxx71 thanks to @aboutcoolscience and @davinci.art
IMMAGINE CC0 CREATIVE COMMONS, si ringrazia @mrazura per il logo ITASTEM. Click here and vote for @davinci.witness
As cancer cells make use of neutrophils to survive and we know it, is there any protocol that can be followed when a former cancer-patient get an infection to prevent the issue? Or maybe is this the topic of the next post? ;)
I think the risk of having circulating cancer cells is higher during the surgical removal of primary cancer and if by accident there is a postsurgical infection (it occurs on average in 40% of the cases) the chances of metastasis are higher. A remedy could be to temporarily lower the platelet count in the patient but the side-effect would be that this patient would be more likely to bleed. If you are interested I can read more about the topic and write a post about it, in the meantime I found an article that discusses this approach: http://www.mdpi.com/2072-6694/9/7/94/pdf
Thanks for the reference. I have quickly browsed it (as you know, my time is limited those days) and it seems that there is again no free lunch. One lowers one risk to increase another one... Feel free to write on this but please don't feel obliged :)
Unfortunately, there are always trade-offs... I am very curious about this topic and I don't mind to read more about it...time is very scarce here lately but I will definitely do it as soon as my schedule clears up a bit, plus some artists made a couple of cool drawings about metastasis that I have to use so another post is going to happen ;) Thank you for your comment!
The trade-off thing seems to be kind of recurrent in our interactions (or is it through the interactions with someone else?) :)
Please don't hesitate to mention me in the next post (I could miss it with my current reduced presence).
If some metastatic cells use platelets as a physical shield, does that mean that drugs like Aspirine which inhibit platelets aggregation can be used for preventive purposes to delay the metastasis ? Do you have any idea if there is any study supporting this claim ?
thank you for your comment, it is not really clear if taking aspirin can significantly lower the chances of metastasis because platelet aggregation is only one of the factors, however here there is a review about this: http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0152402
I can see that there is hope indeed but unfortunately not enough evidence.If someone got cancer and if aspirin has any chance of reducing metastasis , i say he goes for it especially taking low dose aspirine has few drawbacks ! anyway, i enjoyed your article, great work ;)
Thank you!