Mitochondrial medicine: Fact or fiction? Part III – What's the best strategy to deal with mitochondrial dysfunctions?
It's time! It's time for coming to an end with the entire mitochondria discussion. Nevertheless, even after this article, nothing is finished yet. Actually, this is just the beginning. So let's start!
Fig.1: Where is the connection between Spiderman and mitochondria? Nowhere, but somehow everyone thinks there is a connection! Spiderman taken from Pixabay] the other parts are made by Chapper!
We had already learned a lot about our secret masters, called mitochondria. Let's briefly summarize the most important facts:
- Mitochondria are the main energy delivering units within your body [1]!
- Without mitochondria no fatty acids and amino acids/proteins could be consumed for receiving plenty of amounts of energy [2].
- Even sugars could only be degraded with little energy output and thereby increasing the acidification of body in the absence of mitochondria [3].
- Further, no oxygen would be transported by your red blood cells because the mitochondria are involved in the synthesis of porphyrin which is important for this task [4].
- Additionally, mitochondria are bearing many enzymatic steps of the urea cycle and are therefore are prerequisite of detoxification pathways [2].
- In the absence of the controlled cell death carried out by mitochondria your cells would proliferate in an uncontrolled fashion promoting cancer [1-3].
- Not to mention that the transduction of signals in your body. All these mechanisms rely on mitochondria [5, 6].
- Keep in mind that your body forms up to 100 kg of ATP (=energy!) every day and the mitochondria are responsible for up to 90% [7].
- For instance, your cardiac muscle cells (35% of the cell mass are mitochondria) mainly prefer fatty acids [8].
- Eventually, your heart pumps blood through your body and the blood, in turn, consumes the oxygen which is important fort he functions of the mitochondria [9].
- Are your mitochondria not functioning properly, your heart will not functioning properly, which prevents that your entire body will not function properly? [3, 8, 9].
These few facts should make everyone aware of the absolute relevance of the mitochondria for your well-being.
But permanent attacks threaten your mitochondria. As you probably remember, the worst-case is damages within your mitochondrial DNA. These errors have serious effects, especially in the case that cellular recycling mechanisms such as autophagy are malfunctioning. In this case, your body will not be able to remove those flawed mitochondria [10]. Moreover, these mutants replicate and lower your cellular integrity more and more. Especially, in cells such as cardiac muscle cells, this has dramatic consequences [10], due to these areas are not renewed permanently [12]!
But you have to be cautious: malnutrition, stress, toxins, your lifestyle! Anything can hurt your mitochondrial performance. Additionally, besides the direct involvement of the mitochondria many sideshows can have a severe impact.
For many people it is probably not important today, and maybe not tomorrow, but eventually the problems will arise and then you would ask: 1) What is going on and 2) what should be done?
In many cases, therapeutic interventions with various drugs will be carried out. Nevertheless, this often causes more trouble than you had before. The reason is that the true origin of your problem, hidden deep inside your cells is not been seen and therefore untouched...............
Let's face the fact that mitochondria are real! No one can deny their existence or their influence in our lives. But which doctor ever recommended to you for looking up how healthy your mitochondria are? Have you ever talked to someone who told you about mitochondria (except your biology teacher)? Often you hear about problems with the heart, digestion disorder, problems to concentrate, mental problems, fatigue, burnout, depression ... whatever. But did you ever realized that at the basis of all physiological functions cells and with them mitochondria are present?
I have recently looked for mitochondria in the book "Hammer-Examen". Medical students have to read and memorize it at the end of their university career, before becoming doctors. [13]. I realized that the term "mitochondria" can be found at just one in 2,200 pages. In a table, they listed three diseases connected to mitochondria. Please remember that we defined seven categories that could affect mitochondrial health.
Nonetheless, the question remains how you can get a better inside into mitochondrial health? Unfortunately, for most of you, it could be difficult to get their mitochondria examined. Reasons are, for instance, the lack of mitochondrial diagnostics in most laboratories, the low awareness of this subject, the low level of training of doctors in this context, as well as the many question marks around this area.
For keeping it a bit more simple, I would suggest that we concentrate on three major points.
-
Sequencing of mitochondrial genome & measurement of the number of mitochondria in certain cell types
-
Determination of the ATP content within cells
-
Measurement of oxygen consumption and acidification
1. DNA sequencing and determination of the number of mitochondria
DNA sequencing is in principle no brand-new innovation. In the meantime, however, efficiency, sensitivity, and reliability has became better and better. The most sophisticated approaches are for instance Illumina Dye Sequencing or Nanopore Sequencing. I for my part, however, have the opinion that even the outdated Sanger sequencing is still a perfect method [14]. The reason is the acceptable error rate of about 7%, which can be tolerated for our purposes [15]. If you would have a lot of mutations within your mitochondrial genome even the Sanger sequencing will find them. Nevertheless, if you want to sequence your entire genome the Sanger sequencing is not an option.
In Fig.2 you get an impression of how a sequencing might look like. It is a sequencing I did a couple of years ago. I cloned and recombined a gene of choice and finally used the Sanger sequencing to check whether no mutations are present.
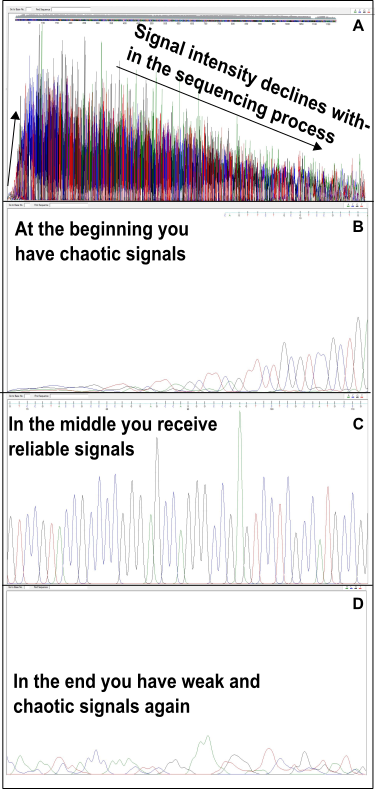
Fig.2: DNA sequencing according to Sanger. (A) Overview. (B) In the beginning, it is rather difficult for DNA polymerase to come into action from a specific starting point (primer). (C) Then you get nice signals. (D) However, the signal intensity decreases rapidly and more and more errors occur. Made by Chapper - unrestricted use allowed.
As you can see there are strong variations in the beginning and at the end. Anyway, it is getting better in the middle part of the sequence. This is because of the fact that the DNA polymerases used for sequencing need a lot of trials to start and gets weak at the end. With overlapping primer pairs, however, you also get information from the start and the end. To realize this you have to clone the DNA into a circular vector. The constant pattern in the middle is of huge importance because you have to make sure that heterogeneous signals are in fact caused by various mitochondrial DNA sequences and not by technical problems.
The most difficult part are the bioinformatics afterwards. Here you need to align all fragments of your sequencing to achieve a comprehensive picture. That means you have to compare all fragments obtained with each other and make statistic predictions about the frequency of a particular mutation. That's not that easy. On average, in my experience, you have a reliable read of about 500 to 800 bp. As you remember, the entire Mito genome is about 17,000 bp in size. Therefore, you have to carry out about 30 sequencing reactions (in case of the Sanger sequencing) to catch all areas appropriately.
To choose the right cells is the next challenge. Cells of the blood, such as lymphocytes, are particularly suitable [16]. It is easy to receive them by a simple blood sample. Because of their remaining telomerase acitivity (check out here and here) they are always "fresh", renewed and in principle immortal. In fact, such a situation doesn't hold true for the entire body (think of the cardiac muscle cells for instance). Additionally, the mitochondrial activity of cells like lymphocytes is little in comparison [7, 10, 11, 16]. Keep in mind that mitochondria are the main source of oxidative stress. The higher the mitochondrial activity the more mutation in the mitochondrial genome can occur. The best view on your mitochondrial situation you will, therefore, get from cardiac or skeletal muscle cells, liver cells, neurons or cells of the kidneys (high mitochondrial activity, low renewal rate) [2, 3, 9, 11]. But, I guess you are not that happy about having a liver or muscle biopsy. This makes the blood cells, in turn, to the most appropriate cells. At least they give you a rough insight into the mitochondrial basic constitution within your body. In addition, these cells naturally floating around in all parts of the body. Maybe they are acting as a mirror of all the scenes they encounter!?!
The ratio of mitochondrial DNA (mtDNA) to nuclear DNA is another important aspect. With a simple qPCR reaction you can easily figure this out. The result has a lot of value due to the average mitochondrial count differs from cell type to cell type [17]. Further, I assume that if too many mitochondria are present within your cells, the performance per mitochondrion is probably insufficient.
2. Determination of cellular ATP
These are tested offered by various companies. However, I often have some problems to see the diagnostic value of such tests. For instance, what does the ATP level of a cell actually tells me? How to discriminate between the ATP generated from mitochondria or glycolysis? Which amounts of ATP are sufficient? Are there certain conditions where the cell of choice maybe don't need that much ATP? Or are there conditions where a high levels of ATP indicates problems? Some companies even take neutrophil granulocytes for such examinations [11]. Neutrophil granulocytes (now called Neutrons by me) are pretty cool cells from the blood because they are behaving like Spiderman but they are no lymphocytes.
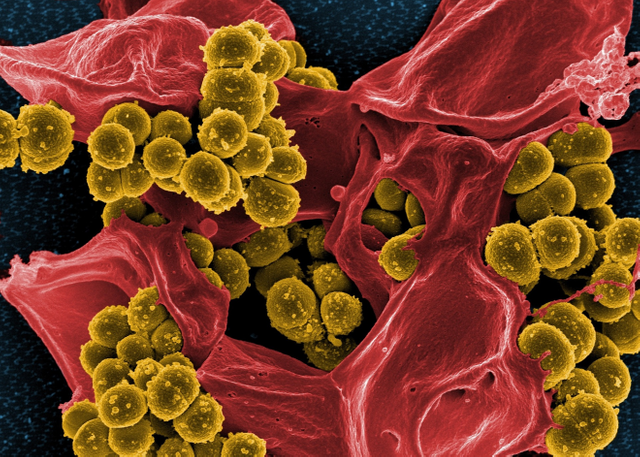
Figure 3: Very nice photo I found on Pixabay. I just searched for "Neutrophils" and then it was suggested to me. I think it is possible to imagine (without knowing more about the origin of the picture) that the NETs (see text below) are the red mucus and the bacteria (here supposedly Staphylococcus aureus) are the yellow-green bobbles. But even if the situation is completely different, the reader will be able to get a good insight into the work of neutrophile granulocytes. Nevertheless, the reader must know that these things have nothing to do with the topic discussed in this article! Neutrophile granulocytes have little to no mitochondrial activity. Unfortunately, many companies offering tests with NeutI have no idea why because Neutrophile granulocytes don't use their mitochondria for energy production! Picture is by Pixabay and thus *** copyright-free.
When the Neutros encounter bacteria, they burst and catching the bacteria into so-called NETs (neutrophile extracellular traps). The NETs prevent that the bacteria can escape thus they will be "frozen" until the cavalry (T cells = lymphocytes, e.g.) arrived [18]. As great as the Neutros are, they produce almost no mitochondrial ATP [16, 19].
But why are some companies using them for mitochondrial testings? I have no idea!It is therefore extremely important that the cell type for ATP determination is well chosen. Lymphocytes or PBMC would be more suitable than neutrophil granulocytes [16]. Platelets are also suitable. Especially since platelets are regarded by some authors as a mirror of the brain [20]. In the end, it is important that you understand what ATP values are telling you. Some companies poison their cells with cyanide, then remove it and finally measure how much ATP can be restored [11]. I don't really know what the output of such test should tell me. You need to know that cells can compensate for a lack of mitochondrial ATP supply by increasing the ATP production via glycolysis and other pathways.
The ratio of ATP to ADP and AMP is another valuable parameter (see Fig.10 here and scroll down here). As you already know, your cells should definitely prevent to form too much AMP. The more AMP accumulates the less ATP is present and the less is the chance to regenerate ADP from AMP. But ADP is important to create ATP. The cell will suffer an energy crisis [7].
The result: ATP depletion!
Keep in mind that you need up to 100 kg ATP per [7].
One reason for elevating the AMP level are the activity of adenylate kinases [21]. Adenylate kinases are using two ADP for converting them into one ATP and one AMP. This happens in the case that the cell is not feasible to generate enough ATP. To have knowledge about such things is at least so important as the knowledge about the amount of mitochondrial and glycolytic ATP.
3. Measurement of oxygen consumption and acidification
Both parameters are very good indicators for cellular performance. Your mitochondria take oxygen to create a lot of energy and acid is often a sign for increased anaerobic glycolysis which produces only little amounts of energy. If the pH value decreases lactate is often responsible. Lactate is, in turn, created in the glycolysis but only if the mitochondria are not able to get the pyruvate before it is reduced to lactate (please see the scheme here again). Therefore, increased acidification is a signal that the metabolic network is somehow inefficient.
A very good approach to measure oxygen consumption is the use of a Clark electrode. Acid produced in the form of lactate can be determined by using specific assays, via chromatography (e.g. HPLC) or spectroscopy (e.g. mass spectrometry).
For a few years, devices exist which can detect oxygen consumption and acidification at the same time, in real-time. Of course, a distinction between lactate and other acids is not possible. However, the benefit of devices such as Seahorse that you can inject various substances or inhibitors and figure out how the cells respond.
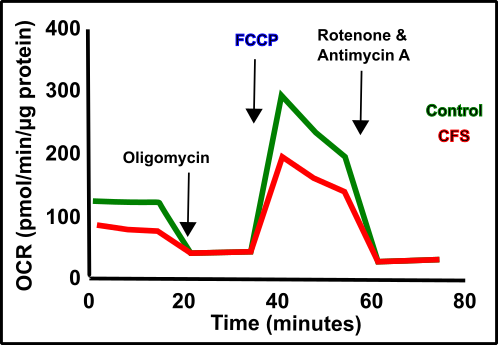
Fig.4: Oxygen consumption (OCR = Oxygene Consumption Rate) in patients with CFS (Chronic fatigue syndrome) compared to healthy patients (the higher the OCR, the more oxygen is consumed, the "better" the mitochondria). The maximum oxygen consumption is triggered by the decoupling of the mitochondrial respiratory chain after the addition of FCCP and referred to as spare capacity. Homemade by Chapper with Data found in Tomas et al. 2018 [22] (CC BY 4.0).
How to imagine a "seahorse analysis" can be seen in Fig.4. Patients suffering from CFS were compared to healthy individuals [22]. CFS stands for Chronic Fatigue Syndrome and is a disease that has been declared as a mental problem for decades. In recent years, however, it has become more and more obvious that bioenergetic problems and therefore also mitochondrial problems could be responsible for CFS. People who are suffering from such things are quickly exhausted mentally and physically. Depending on the severity, CFS patients often are unable to do even trivial things such as washing the dishes without complete exhaustion. In Fig. 4 you can see that CFS patients appear to have a very spare capacity. The spare capacity can be determined after FCCP injection. You probably remember that your mitochondrial membrane works like a battery (Fig.5).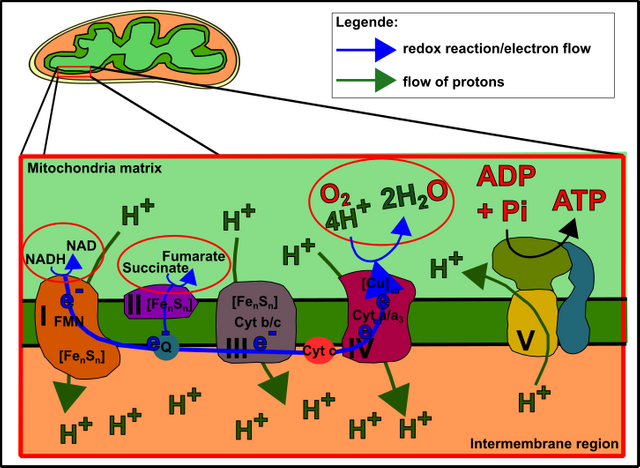
Fig. 5: The mitochondrial respiratory chain. Electrons from food are transferred to the respiratory chain. This drives proton pumps. The separation of charges creates (protons are positively charged) voltage. Eventually, the "battery" is discharged via complex V (ATP synthase) and thus produces ATP. Made by Chapper - unrestricted use allowed.
Note: Check my "gif story" about mitochondrial function right here for better understanding.
On the mitochondrial membrane, charge separation is carried out by proton pumps. These proton pumps, in turn, are powered by electrons, which are provided by the food you consume. The stronger the charge separation, the more work is needed to pump protons. In the end, the electrons are transferred on oxygen which is reduced to water (that's why we need air!). The addition of FCCP decouples this mechanism because FCCP transports the protons back across the membrane. As a result, the gradient collapses every time and electrons are transferred to oxygen rapidly to reestablish the gradient. This leads to increased oxygen consumption (Figure 6).
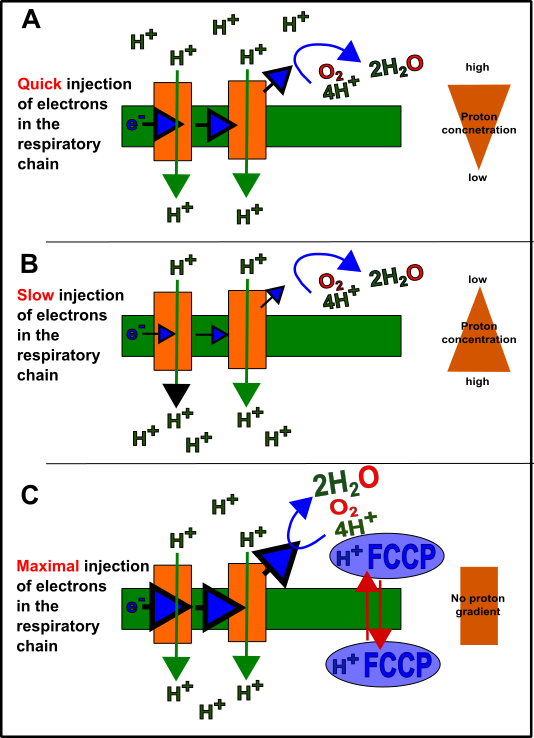
Fig.6 Theory behind electron flow, oxygen consumption and decoupling by FCCP. In case that the mitochondria have only little activity many protons are present at the matrix side (A). In general, the mitochondria work sufficient shifting the majority of protons to the intermembrane side (B) through the work of the proton pumps. The protons, as shown in Fig. 5, later flow back via the ATP synthase (complex V) and thus supporting the generation of ATP. Due to the increased voltage, the flow of electrons is "slowed down" a bit because it has to resist against this gradient. (C) FCCP decouples this equilibrium by transporting protons undirected across the membrane. As a result, the electrons have no backpressure and therefore result the maximal oxygen consumption rate which can be used to calculate the spare capacity. Made by Chapper - unrestricted use allowed.
It is probably obvious that the spare capacity (i.e. the maximum possible oxygen consumption) depends strongly on an intact respiratory chain. As we saw in Figure 5, as well as in the first two parts of this series Part 1 & Part 2, is that the respiratory chain is built out of various components or factors. Many of these factors are encoded in the mitochondrial genome (DNA, Fig.8 here). But not only the factors of the respiratory chain are important. Also, the supply of the reduction equivalents, transferring the electrons from the food to the chain, is crucial. See also my other articles for more information here. Even the relative position of the components the respiratory chain is made is a critical aspect of the electron flow. A really great article on the topic was recently published in Cell [23]. Just click on the link and scroll through the document, where you can see that the complexes are organized in some kind of super complex, also known as Respirasom. The mitochondrial function therefore also depends on the formation of this Respirasom. And this aspect is probably far above the usual assumptions such as mitochondrial DNA quality.
Anyway. Fig.4 shows that CFS patients do not perform as well as healthy persons. Nevertheless, it is questionable whether this is the cause or the consequence of the disease. Moreover, the question is what causes the decreased spare capacity: Mutations within genes? Low electron supply from other pathways? A damaged respiratory chain? Weak respirasom formation? Low numbers of mitochondria...??? Further, it should also be clarified whether this can be correlated with the physical and mental performance of people. Unfortunately, this is only insufficiently answered by the study.
This fact suggest that additional testings are absolute important making the diagnosis of mitochondrial dysfunctions becoming a hard task.
Further examination could be the measurement of the glutathione content (see Figure 5 here). Further, you can measure the formation of reactive oxygen species (ROS), as well as the resulting peroxides. And of course ATP measurement, sequencing, mitochondria number... I guess you understand what I mean!
In patients with an unclear clinical pattern, a combination of different tests is absolutely necessary. In contrast, in patients who suffer from MELAS or MERFF (see Part 2 again) DNA sequencing will probably after answer the most urgent questions. Nevertheless, even patients with genetic mutations can live normally in case that the cells are able to compensate defects (please see my article about LHON here for more).
The big question mark is the therapeutic consequence.
And to be honest, I can not finally answer this. Moreover, you should always be critical if someone offers the ultimate treatment strategy for these sicknesses. In fact, most serious publications on the subject currently have either no [24] or only limited suggestions to cure [11, 13, 25-28] such issues.
Let's check out some possibilities:
1. Activate autophagy: I will not go into detail now. The reader of my blog already knows it and everyone else is recommended to read my articles on this subject. Interesting in this context is the fact that diseases like LHON get worse over with age [24, 29]. Does this mean that there are a few fit mitochondria left that are somehow removed over time? I don't know! Nevertheless, of course, anyone can try to be a good platform to the "super mitochondria" within your cells. How do you could do it, please see here.
2. Reduction of stress: Again, I will not go into detail here, because I did it "a thousand times" before.
3. Optimal Diet: This is something that can be really difficult. Sure, you should, of course, only eat healthy food (read my article here. But whether you should prefer carbohydrates, fatty acids or proteins is a very individual question [30]. In fact, the answer to this question is not as easy as some people suggest. With the Seahorse you can, also figure out which fuels your mitochondria like (my cells are addicted to sugar, by the way). Try to find the optimal diet for you and consult, in case of doubt, a doctor or nutritionist.
Optimal nutrition = optimal energy production = optimal health.
4. Supplementation: We already discussed this several times and you know that I only suggest vitamin D [30]. Nevertheless, coenzyme Q10 (CoQ10) has been shown to partially reduce the problems of LHON patients [28].
CoQ10 is the electron transmitter between Complex III & IV of the mitochondrial respiratory chain (the Q in Fig. 5 above). Of course, your body produces this by itself, but sometimes not in sufficient quantities. Since it is fat-soluble, you must either eat it in a fat-soluble emulsion or together with fatty foods [31]. Supplementing CoQ10 seems safe, but may increase the risk of internal bleeding, headache, or allergies, for instance [25]. The question is, of course, whether the bioavailability is high enough that you might have a benefit by supplementing it. In this context, it has been shown that bioavailability depends on the dosage form of CoQ10 [32].
There are also approaches to supplement glutathione. You already know from Part 1 of this series that the glutathione system is responsible for counteracting oxidative stress. To do this, it works together with vitamin C and E [33]. Nonetheless, to my knowledge, there is no carrier for glutathione to bring it into the cells. Only carriers to release glutathione are known, which is important for detoxification [34]. Anyway, it is important to understand that the formation of glutathione is closely connected to folic acid [24]. A sufficient supply of folic acid, therefore, is a good way to strengthen the glutathione system.
Other measures include sleep, exercise, and general well-being. I also read in an article that a stone age diet, chelator therapy, and infrared saunas could help [27]. Ok, the stone age diet will definitely make sense [30]. Even with the chelators, I agree, because of these substances are binding heavy metals, which in principle could cause oxidative stress, also inhibit your enzymes and do a lot of other worse things (see also here). In the case of infrared saunas, however, I have no idea about the mechanisms. That would be something for a new article.
Alright, I think that's enough for the topic. I hope I could bring you closer to the meaning of mitochondrial medicine and hopefully draw some conclusions for you personally, which in the future either prevent or at least mitigate some problems.
Due to I reorder my blog, I will probably re-issue old articles first. Further, shorter articles will be produced in the next future.Until then, as always …
Steem On!
Chapper
References:
- Müller-Esterl, W., Biochemie: Eine Einführung für Mediziner und Naturwissenschaftler. 2004: Spektrum Akademischer Verlag.
- Peter Karlson, D.D., Jan Koolman, Georg Fuchs, Wolfgang Gerok, Ruth Hammelehle, Karlsons Biochemie und Pathobiochemie. Vol. Auflage: 15. 2005: Thieme.
- Püschel, Taschenlehrbuch Biochemie. 2011: Thieme Verlagsgruppe.
- Hill, F.E.D.E.D., Porphyrine: Ein Ring für die Farben des Lebens. Spektrum der Wissenschaft Biologie Medizin Hirnforschung, 2019. 1/19.
- Lombardi, A.A. and J.W. Elrod, Mediating ER-mitochondrial cross-talk. Science, 2017. 358(6363): p. 591-592.
- Hirabayashi, Y., et al., ER-mitochondria tethering by PDZD8 regulates Ca(2+) dynamics in mammalian neurons. Science, 2017. 358(6363): p. 623-630.
- Booth, N.E., S. Myhill, and J. McLaren-Howard, Mitochondrial dysfunction and the pathophysiology of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). Int J Clin Exp Med, 2012. 5(3): p. 208-20.
- Park, S.Y., et al., Cardiac, skeletal, and smooth muscle mitochondrial respiration: are all mitochondria created equal? Am J Physiol Heart Circ Physiol, 2014. 307(3): p. H346-52.
- al., G.e., Taschenlehrbuch Physiologie. 2. Auflage ed. 2015: Thieme.
- Hill, B.G., et al., Integration of cellular bioenergetics with mitochondrial quality control and autophagy. Biol Chem, 2012. 393(12): p. 1485-1512.
- Myhill, S., N.E. Booth, and J. McLaren-Howard, Chronic fatigue syndrome and mitochondrial dysfunction. Int J Clin Exp Med, 2009. 2(1): p. 1-16.
- Kikuchi, K. and K.D. Poss, Cardiac regenerative capacity and mechanisms. Annu Rev Cell Dev Biol, 2012. 28: p. 719-41.
- Buchta, e.a., Das Hammerexamen: Repetitorium für den 2. Abschnitt der Ärztlichen Prüfung. Vol. Auflage: 2. 2008: Urban & Fischer Verlag/Elsevier GmbH.
- W. Janning, E.K., Genetik: Allgemeine Genetik - Molekulare Genetik - Entwicklungsgenetik. 2004: Georg Thieme Verlag.
- Wang, X.V., et al., Estimation of sequencing error rates in short reads. BMC Bioinformatics, 2012. 13: p. 185.
- Chacko, B.K., et al., Methods for defining distinct bioenergetic profiles in platelets, lymphocytes, monocytes, and neutrophils, and the oxidative burst from human blood. Lab Invest, 2013. 93(6): p. 690-700.
- Robin, E.D. and R. Wong, Mitochondrial DNA molecules and virtual number of mitochondria per cell in mammalian cells. J Cell Physiol, 1988. 136(3): p. 507-13.
- Tillack, K., et al., T lymphocyte priming by neutrophil extracellular traps links innate and adaptive immune responses. J Immunol, 2012. 188(7): p. 3150-9.
- Maianski, N.A., et al., Functional characterization of mitochondria in neutrophils: a role restricted to apoptosis. Cell Death Differ, 2004. 11(2): p. 143-53.
- Torti, I.C.F.G., Platelets in Neurological Disorders, in Platelets in Thrombotic and Non-Thrombotic Disorders. 2017, Springer, Cham.
- Dzeja, P. and A. Terzic, Adenylate kinase and AMP signaling networks: metabolic monitoring, signal communication and body energy sensing. Int J Mol Sci, 2009. 10(4): p. 1729-72.
- Tomas, C., et al., Cellular bioenergetics is impaired in patients with chronic fatigue syndrome. PLoS One, 2017. 12(10): p. e0186802.
- Milenkovic, D., et al., The Enigma of the Respiratory Chain Supercomplex. Cell Metab, 2017. 25(4): p. 765-776.
- Suomalainen, A. and B.J. Battersby, Mitochondrial diseases: the contribution of organelle stress responses to pathology. Nat Rev Mol Cell Biol, 2018. 19(2): p. 77-92.
- Garrido-Maraver, J., et al., Coenzyme q10 therapy. Mol Syndromol, 2014. 5(3-4): p. 187-97.
- Michalak, K., et al., Treatment of the Fluoroquinolone-Associated Disability: The Pathobiochemical Implications. Oxid Med Cell Longev, 2017. 2017: p. 8023935.
- Myhill, S., N.E. Booth, and J. McLaren-Howard, Targeting mitochondrial dysfunction in the treatment of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) - a clinical audit. Int J Clin Exp Med, 2013. 6(1): p. 1-15.
- Viscomi, C., Toward a therapy for mitochondrial disease. Biochem Soc Trans, 2016. 44(5): p. 1483-1490.
- Kirches, E., LHON: Mitochondrial Mutations and More. Curr Genomics, 2011. 12(1): p. 44-54.
- Kast, B., Der Ernährungskompass: Das Fazit aller wissenschaftlichen Studien zum Thema Ernährung - Mit den 12 wichtigsten Regeln der gesunden Ernährung. 2018: C. Bertelsmann Verlag.
- Hernandez-Camacho, J.D., et al., Coenzyme Q10 Supplementation in Aging and Disease. Front Physiol, 2018. 9: p. 44.
- Lopez-Lluch, G., et al., Bioavailability of coenzyme Q10 supplements depends on carrier lipids and solubilization. Nutrition, 2019. 57: p. 133-140.
- Kalyanaraman, B., Teaching the basics of redox biology to medical and graduate students: Oxidants, antioxidants and disease mechanisms. Redox Biol, 2013. 1(1): p. 244-57.
- Ballatori, N., et al., Plasma membrane glutathione transporters and their roles in cell physiology and pathophysiology. Mol Aspects Med, 2009. 30(1-2): p. 13-28.
Posted from my blog with SteemPress : http://worldofchapper.de/rp295320-ovh/index.php/2019/10/03/mitochondrial-medicine-fact-or-fiction-part-ii-whats-the-best-strategy-to-deal-with-mitochondrial-dysfunctions/
Interesting one here. This is my first time of reading your blog. I guess I have a lot to catch up to but I've got a question,
What is the average number of mitochondrion in a human cell? I guess from this, one can easily calculate the average total number of mitochondrion in a human body. I don't know if there are variations and if yes, what are the factors that cause these variations in the number of mitochondrion per cell?
Posted using Partiko Android
Hey @gentleshaid,
thanks for coming by. In fact, depending on the cell type of choice you have variations in the number of mitochondria. Metabolic highly active cells (liver cells or cardiac muscle cells) have thousands of mitochondria per cell. Immune cells (lymphocytes), in contrast, have sometimes less than 100 up to a few hundred mitochondria per cell. The more energy they produce the more mitochondria you need. However, in the neutrophils (also immune cells but almost no mitochondrial ATP) only 5-6 mitochondria are present per cell.
I hope this answers your question
Have a nice weekend
Chapper
Great post! I am glad to see you back (as you had never left)! I have a few questions/comments.
From what you wrote, it seems that there are actually no real way to test the health of our mitochondria, at least for normal people (and it may even be harder for those living in the middle of nowhere). Therefore, I am a bit puzzled. We today know (at least I know thanks to you) that they are super important and could be at the root of many severe health issues. So why can’t we (as humans) pay more attention to that? It sounds a little bit like looking elsewhere when one should focus on the main thing…
At the end of the day, the only option that is left seems to live healthy, which is probably what fewer and fewer people do, to make sure we don/t put it too high on our mitochondria.
I will just comment on this and bring it to my personal case: I moved a month ago to write shorter articles of only about 1000-1100 words. It turned out that I got more and more comments and interactions on my posts. I think that @abigail-dantes got something similar on her side. Maybe this will also help you to get more readers too. I guess we will know soon :)
Hey @lemouth,
the problem is that these findings are somehow "cutting-edge". For instance, look at what Eric Kandel figured out about molecular mechanisms about learning and memory (Nobel prize in 2000) and look at how universities and schools are still organized.
It takes a while until the authorities (and they eventually decide in the end) take note of it and implement it into the routine. Until then everyone should "obey" the proposals at the end of the article (lower the intake of foods, exercise, reduce stress, relax, sleep well). With such "simple" interventions you can (indirect) protect your mitochondria or at least prevent severe damage.
You are definitely right, I also like smaller posts. This one has about 4000 words, which means about 3 to 4 fold larger as the length you suggest. I will try it but sometimes topics are too complex to just put it into a few sentences. On the other hand, it is also a sign of good understanding and skill to put complex issues into a few, simple words.
Thanks for the comment and the suggestions
Have a nice weekend
Chapper
I mistakingly thought this knowledge was old enough to already be applied. I was definitely too naive. Thanks for the update (and correction ;) )!
Unfortunately, not or at least not in Germany for ordinary people.
Posted using Partiko Android
I guess the entire Europe should then be similar...
Might be!
I do, I do! :) It works well.
Ich danke für herzlich für diesen starken Beitrag!
Muss mich gleich nochmal nach Part 1 umschauen.
Du hast dir sehr viel Mühe gemacht und alles ausführlich und gut verständlich erklärt.
Danke, dass du dir so viel Mühe gemacht hast.
Beste Grüße
Lindi
Posted using Partiko Android
Hi vielen Dank für deine Antwort! In der Tat macht dies viel Arbeit. Es ist allerdings schon der dritte Teil, ist mir dank deines Kommentars erst aufgefallen. Beste Grüße
Posted using Partiko Android
Ach, siehst du mal! Dann schaue ich mich natürlich nach Part 1&2 um ;)
Posted using Partiko Android
🤣👍😁 viel Spaß!
This post has been voted on by the SteemSTEM curation team and voting trail. It is elligible for support from @curie and @minnowbooster.
If you appreciate the work we are doing, then consider supporting our witness @stem.witness. Additional witness support to the curie witness would be appreciated as well.
For additional information please join us on the SteemSTEM discord and to get to know the rest of the community!
Please consider using the steemstem.io app and/or including @steemstem in the list of beneficiaries of this post. This could yield a stronger support from SteemSTEM.
Thank you guys! 👍
Für die LHON ist seit 2015 eine Therapie mit Idebenon in Deutschland zugelassen - auch wenn Raxone - ähnlich Coenzym Q10 - wirkt und den primären Endpunkt seiner Zulassungsstudien nicht erreichte, so ist wegen der guten Ergebnisse bei den sekundären Endpunkten eine Zulassung bei der LHON erfolgt.
Insofern ist der Beitrag im Hinblick auf die Ausführungen zur LHON nicht auf dem neuesten Stand, was aber den insgesamt qualitativ hochwertigen Ausführungen und dem darin enthaltenen Erkenntnisgewinn keinen Abbruch tut - ganz im Gegenteil.
Hast es geschafft, dass ich mich vier Stunden lang durch wissenschaftliche Datenbanken gefortstet habe und mir vieles neues reingepfiffen habe - und das am Sonntagnachmittag.
Deine Artikel sind echt teuflisch gut. Hut ab und ganz lieben Dank für die Einblicke, die Du uns in Chappertons Welt der Mitochondrien gewährst.
SEND with LOVE.
Peace.
Hey @indextrader24,
genau aus diesem Grunde mache ich die Artikel. Ich sagte bereits zu @kadna, dass ich dabei etwas lernen will und, was soll ich sagen, dank dir ist mir das wieder gelungen. Nun hast du mich nämlich dabei unterstützt mehr über Therapiekonzepte in Erfahrung zu bringen. Ziel erreicht!
In dem Sinne freue ich mich natürlich gern wieder, wenn du bei mir vorschaust und freue mich, dass ich dich derart zum Nachdenken und Nachforschen anregen konnte.
Vielen Dank für die Blumen
Beste Grüße
Chapper
Hallo Chapper,
so befruchten wir uns gegenseitig. Gern geschehen, denn der Dank ist ganz meinerseits, denn auch ich habe dazugelernt.
Zumal das Thema, was Du anschneidest, in der klassischen Schulmedizin eher ein Schattendasein führt und eigentlich wesentlich stärkere Betonung erfahren sollte.
Herzliche Grüße.
SEND with LOVE!
Hi, @chappertron!
You just got a 0.28% upvote from SteemPlus!
To get higher upvotes, earn more SteemPlus Points (SPP). On your Steemit wallet, check your SPP balance and click on "How to earn SPP?" to find out all the ways to earn.
If you're not using SteemPlus yet, please check our last posts in here to see the many ways in which SteemPlus can improve your Steem experience on Steemit and Busy.
Wundert uns das?
Ursachenforschung ist nicht opportun - sie würde die Lebenserwartung des Einzelnen deutlich verlängern und das sozialverträgliche Frühableben drastisch reduzieren was natürlich ökonomisch im Sinne der Sozialisten nicht erwünscht sein kann, weil damit die Machtansprüche in Frage gestellt werden.
Gesundheitssozialismus findet sich somit auch im staatlichen Bildungsbetrieb.
Toller Beitrag.
Hallo @janasilver,
was auch immer die Beweggründe im einzelnen sind (kann ich aufgrund mangelhaften Wissens darüber nicht beurteilen), ich hoffe, dass ich mit der Wissensvermittlung, zu diesen Themen, viele Leute erreichen konnte. Die Mito-Medizin ist ja auch kein HokusPokus sondern harte Naturwissenschaft, und seit Jahrzehnten bewert. Immerhin gibt es mittlerweile viele Therapeuten, die sich dieser Problematik widmen, irgendwann wird man aus wirtschaftlichem Interesse einfach folgen müssen.
Ich schaue also optimistisch in die Zukunft und bis dahin schreibe ich stoisch mein Zeug hier weiter.
In diesem Sinne
Steem on Da Mitos ;-)
Servus,
eine kleine Anmerkung noch - die Sache mit der maternalen Herkunft der mt-DNA scheint inzwischen überholt zu sein.
https://steemit.com/deutsch/@indextrader24/wichtige-aspekte-mitochondrialer-sehnervenerkrankungen-stammt-die-mitochondriale-dna-mt-dna-auch-vom-vater
Beste Grüße!
!COFFEEA
Hi Silver, dies ist durchaus richtig. Doch werden paternale DNAs zumeist schnell durch die Mitophagie beseitigt und spielen somit im erwachsenen Lebewesen keine Rolle Mehr.
https://www.nature.com/articles/d41586-019-00093-1
Gruß
Thank you very much!